Robotic/ Thoracoscopic Surgery for Myasthenia Gravis
Myasthenia Gravis surgery generally involves procedures designed to address the root causes or alleviate the symptoms of this neuromuscular condition.
What is Thorascopic?
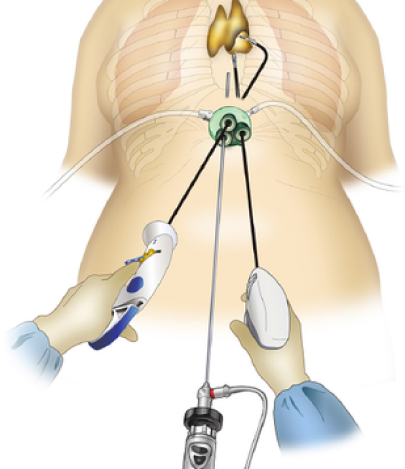
Robotic and thoracoscopic surgery offers a cutting-edge, minimally invasive approach to treating Myasthenia Gravis (MG), a chronic autoimmune condition that affects neuromuscular transmission. These advanced surgical techniques are particularly effective in performing thymectomy—the removal of the thymus gland, which plays a central role in managing and potentially improving symptoms of Myasthenia Gravis. With the use of robotic-assisted systems and thoracoscopic technology, this procedure ensures precision, minimizes surgical trauma, and reduces recovery time, enhancing patient outcomes and quality of life.


Symptoms and Digonosis
Muscle Weakness:
The hallmark symptom of MG is muscle weakness that worsens with activity and improves with rest.
Ptosis (Drooping Eyelids)
Weakness in the eyelid muscles can cause drooping of one .
Difficulty Swallowing
The muscles involved in swallowing may weaken, making it difficult to swallow food .
Treatments
Surgery

Medicnine

Dietary Changes

Myasthenia Gravis
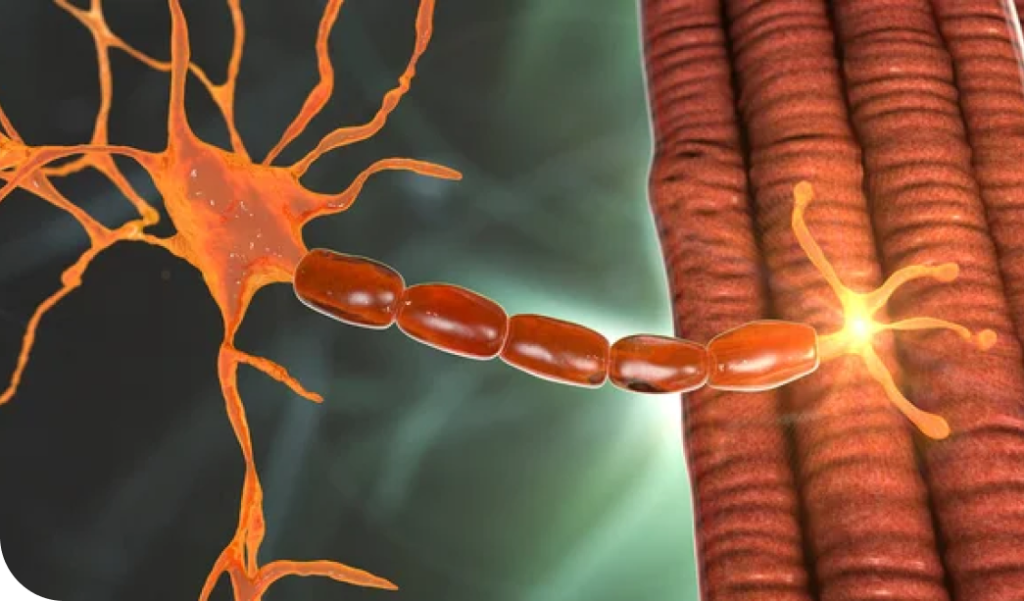
Myasthenia Gravis (MG) is a chronic autoimmune disorder that affects the nervous system and causes weakness in the voluntary muscles. The condition occurs when the body’s immune system produces antibodies that block or destroy the receptors for acetylcholine, a neurotransmitter that is essential for transmitting nerve signals to muscles. As a result, the affected muscles do not receive the necessary signals to contract properly, leading to muscle weakness.
Surgery
Surgery for Myasthenia Gravis (MG) primarily involves thymectomy, the removal of the thymus gland. The thymus is believed to play a role in the abnormal immune response that leads to MG.
Characteristics of Myasthenia Gravis:
Robotic or thoracoscopic thymectomy involves the following steps:
1. Pre-Operative Evaluation: Detailed imaging studies, including CT or MRI, help assess the thymus gland and surrounding structures.
2. Minimally Invasive Access: Small incisions are made on one or both sides of the chest to insert a thoracoscope (a small camera) and robotic instruments.
3. Thymus Removal: Using advanced tools and high-definition imaging, the surgeon meticulously removes the thymus gland, including any associated tumours.
4. Closure: Incisions are closed with sutures or adhesive for minimal scarring. The procedure is performed under general anaesthesia and typically takes 2-3 hours.

Bala
"Before my surgery, I had severe weakness in my arms, legs, and face, and simple tasks like walking or talking would exhaust me. My doctor recommended a thymectomy, and I underwent minimally invasive surgery. The recovery was quicker than I expected, and within a few months, I noticed significant improvements. I’m now able to live a more active life, and I’ve been able to reduce my medication. I’m so thankful for the surgery and the care I received."

Susan
Sed ut perspiciatis unde omnis iste natus error sit voluptatem accusantium doloremque laudantium, totam rem aperiam.
John
Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.